Inside Neuroscience: How the Brain Reacts to Stress
"These days, stress is one of the most commonly used words in the English language,” said Bruce McEwen, head of the Harold and Margaret Milliken Hatch Laboratory of Neuroendocrinology at Rockefeller University and moderator of a Neuroscience 2017 press conference on the effects of stress on the brain.
“Good stress” does exist, but when most of us think of stress, we think of “bad stress,” which has negative consequences when uncontrolled. That kind of stress is pervasive in our lives — from the little day-to-day stressors we all face to major life events such as the loss of a loved one or job to the traumatic experiences of some children, soldiers, and others. Some of these stressors are tolerable, but others are toxic and can accelerate disease processes in the body as well as the brain.
While it’s well known that chronic stress can cause or exacerbate neurological, systemic, and mental health disorders, as well as predisposition to disorders developed later in life, the mechanisms by which this happens are still relatively unknown. Research presented during the press conference aims to deepen our understanding of the neurological effects of stress and improve our ability to address and potentially reverse its negative effects. In this research, high or prolonged elevation of levels of cortisol, a glucocorticoid hormone, plays an important role, although it is important to remember that cortisol, when not in excess, also has many positive effects that are necessary for normal function, adaptation, and survival.
Identifying a Biological Record of Trauma
Childhood trauma can cause long-term health and behavioral issues such as post-traumatic stress disorder (PTSD), so early detection of trauma is critical for preventing further abuse and addressing these negative consequences. To determine whether trauma is accompanied by potential biomarkers that may be used to identify young victims of child abuse, a group of researchers at the University of New Mexico Health Sciences Center studied children who suffered trauma and were undergoing cognitive behavior therapy to see whether the trauma had triggered long-term, persistent epigenetic changes.
The researchers explored the missing link between DNA methylation, a reversible biochemical process that turns genes “on” or “off” by adding a methyl group to a DNA sequence, and prolonged elevated cortisol levels, a bodily response to long-term stress that may potentially change the methylation process and thereby gene expression. By comparing cortisol levels measured from samples of the children’s hair and DNA methylation patterns in saliva, the researchers confirmed this relationship.
“We found 174 genes altered in traumatized children with elevated cortisol,” study co-author Brianna Mulligan said. “These are whole-body, global changes.”
The researchers are now working on a new silicon chip that can detect methylation changes in real time, which could be used to identify patients whose bodies are undergoing epigenetic changes. Identifying the timing of changes in methylation patterns may help to guide early interventions and inform new treatments for PTSD.
Astrocytes’ Role in Fear Response After Stress
Neuroscientists at the University of North Carolina at Chapel Hill have found a connection between astrocytes, specialized glial cells vital to brain function and health, and the brain’s hyper-reactivity to fear following exposure to stress.
Cortisol is not the only mediator involved in effects of stress. Previous work has shown that preventing the release of a particular protein connected to the brain’s response to stressors, interleukin-1β (IL-1β), prevents the development in animals of symptoms similar to those of PTSD. By directly manipulating astrocytes, which produce stress-induced IL-1β, the scientists were able to prevent its release, manifesting as a reduction in fear and anxiety. This effectively established a relationship between astrocytes and stress response and brings researchers closer to understanding the neurobiology of PTSD.
“Our data suggest that astrocyte signaling alone is sufficient to influence how a stressor changes the way that animals learn about fear,” said Meghan Jones, lead author of the study. “This would suggest that looking at the function of astrocytes in the context of human PTSD might ultimately help us help people better.”
How Dad’s Stress May Affect His Offspring
Stress can affect not only an individual’s brain but also the brains of his or her offspring. In a famous study conducted in Överkalix, Sweden, researchers found that grandfathers who lived through times of famine had grandsons who lived longer than those of grandfathers who lived in times of plenty. Inspired by this study, scientists at the University of Pennsylvania set out to investigate how a father’s stressful experiences may alter the gene expression of his sperm.
“One question that hasn’t been addressed is: How do dads’ experiences change their germ cells? What is the sensor in dads’ reproductive tract that can detect the changes in environment and translate that to epigenetic programming in the sperm?” said Jennifer Chan, lead author of the study.
The caput epididymis, where sperm matures, appears to serve an important function in this process. In times of stress, the researchers saw increased levels of glucocorticoid receptor (GR), a gene regulator, in the caput epididymis and postulated that GR changes the programming of microRNA in the sperm and thus gene expression in offspring.
To test this hypothesis, the researchers induced stress and then reduced GR levels in the epididymis of adult male mice. This normalized the dysregulated stress response in the offspring, indicating that GR may in fact be an important mediator in the creation or modification of sperm microRNA at this critical stage. Future research will be aimed at finding an RNA signature in sperm that indicates previous toxic stress exposure in humans.
The Power of Neurogenesis to Reduce Stress
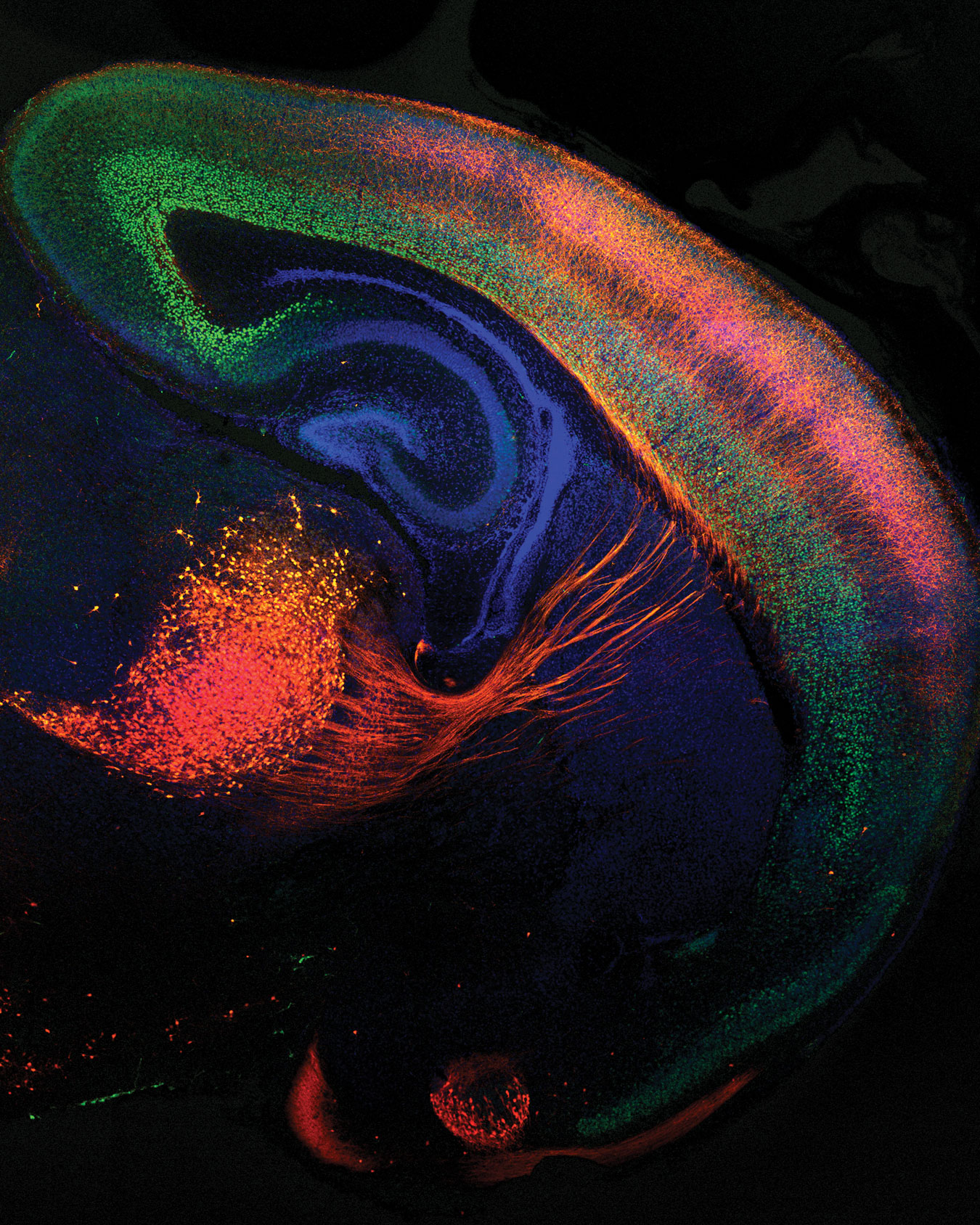
The hippocampus, the region of the brain where fear learning takes place, is sensitive to the effects of stress, and it is capable of considerable structural plasticity, including neurogenesis, in response to experiences, including stressors. Researchers at Columbia University have been exploring whether stimulating neurogenesis, or the creation of new cells, in the hippocampus can make the brain more resilient to negative effects of stress.
Mice that were genetically modified to produce an abundance of new hippocampal cells showed less activity in the hippocampus in response to chronic stress and therefore less anxiety. The opposite was also true: When exposed to stress, mice genetically modified to have fewer new hippocampal cells exhibited more activity in stress-responsive cells, resulting in greater anxiety. Using miniature microscopes attached to the heads of the mice, the researchers observed activity inside the mouse brain to prove that this increased cell activity occurred simultaneously with a stressful experience, providing novel insight about the causal relationship between neurogenesis and stress response.
According to the researchers, activities that promote neurogenesis, such as physical exercise, and living in an enriched environment can be encouraged for certain patients, and medication could be developed to affect the hippocampus directly. “New antidepressant targets could be developed to increase new brain cells or directly silence stress-responsive cells,” said Christoph Anacker, lead author of the study.
Stress-Fighting Bacteria
The combination of sleep deprivation and stressful experiences is a “double hit” that increases our potential vulnerability to toxic stress; however, Northwestern University researchers have discovered that Mycobacterium vaccae, a harmless bacterium found in soil, can buffer against these negative effects in mice.
When researchers exposed mice to the double hit of sleep deprivation and stress, the mice were unable to learn a task. When the researchers injected the mice with the bacterium before exposure to the double hit of sleep loss and stress, however, the mice exhibited stress resilience and were able to learn the new task. The data suggest that the bacterium helps to modulate inflammation, showing promise for microbial-based immunity as a potential therapeutic target. As a part of the “hygiene hypothesis,” the research also supports the idea that less exposure to “beneficial” bacteria like M. vaccae may contribute to maladaptive neurobiological responses characterized by excessive inflammation. Future research will delve more deeply into this idea and investigate possible interventions involving bacteria.
“Studying the gut bacteria and bacteria in our environment that we call ‘old friends’, that we’ve coevolved with . . . as potential therapeutic targets holds potential for prevention and treatment for psychiatric and neurobiological disorders,” researcher Samuel Bowers said.
The Brain Is a Dynamic Organ
Collectively, these studies contribute to our growing understanding of the ways in which the brain responds to stress, with concurrent effects on the body. “The brain used to be regarded as an invariant organ after birth, but we now know it is dynamic in its structure and function and experiences adaptive plasticity but also is vulnerable to insults,” McEwen said.
While toxic stress cannot be prevented entirely, it can be made more tolerable if we better define the relationships among stress, the brain, and systemic physiology. Understanding these relationships can then lead to strategies for mitigating both its immediate and long-term effects.