The Changing Face of Post-Traumatic Stress Disorder
- Published20 Jun 2019
- Author Alexis Wnuk
- Source BrainFacts/SfN

Our understanding of the emotional toll of war is likely as old as war itself. What we now know as PTSD has gone by many names over the last four centuries, but its recognition as an official diagnosis in 1980 changed how we think of trauma.
What’s in a Name?
In William Shakespeare’s Henry IV, Part 1, Hotspur returns from battle a changed man. His wife, Lady Percy, inquires in a well-known soliloquy: “In thy faint slumbers I by thee have watched, / And heard thee murmur tales of iron wars.” Shakespeare described a constellation of symptoms that would go by many names over the next 400 years — soldier’s heart, shell shock, battle fatigue. Its formalization into a psychiatric diagnosis — post-traumatic stress disorder — in 1980 was a watershed moment for our understanding of trauma, affirming that traumatic experiences could have enduring consequences for brain function and mental health.

“The challenge … for military medicine was how to explain how a soldier could be totally incapacitated when there was no blood, no broken bones, no fever, no obvious sign of any physical problem,” says Matthew Friedman, former executive director of the National Center for PTSD.
Recognizing the need for a common language to diagnose and treat mental disorders, the American Psychiatric Association published the Diagnostic and Statistical Manual of Mental Disorders in 1952. It included a diagnosis called gross stress reaction, an overwhelming fear response brought on by the extreme emotional or physical stress of combat or a natural disaster.
For reasons that aren’t clear, the term was omitted from the second edition of the DSM in 1968.
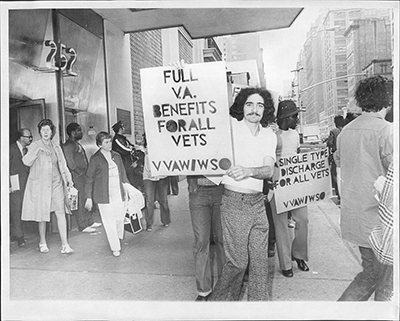
This proved consequential as soldiers returning from Vietnam organized and clamored for a diagnosis recognizing the psychological impact of war. At the same time, clinicians realized stressful experiences like natural disasters and domestic abuse could similarly affect mental health. The DSM-III, published in 1980, introduced a term encapsulating all these experiences: post-traumatic stress disorder.
Unraveling the Neurobiology
The PTSD diagnosis fundamentally changed our understanding of trauma. It recognized “that a psychological event can produce profound if not enduring alterations in brain function, behavior, emotional regulation, and cognition,” Friedman says. According to the DSM-III, anything “outside the range of usual human experience” — such as combat, rape, assault, torture, natural disasters, and accidents — qualified as a traumatic experience. The definition also recognized that symptoms could be chronic and that preexisting mental health problems increased someone’s odds of developing PTSD — a departure from earlier criteria for gross stress reaction that specified symptoms were short-lived and occurred only in previously normal individuals.
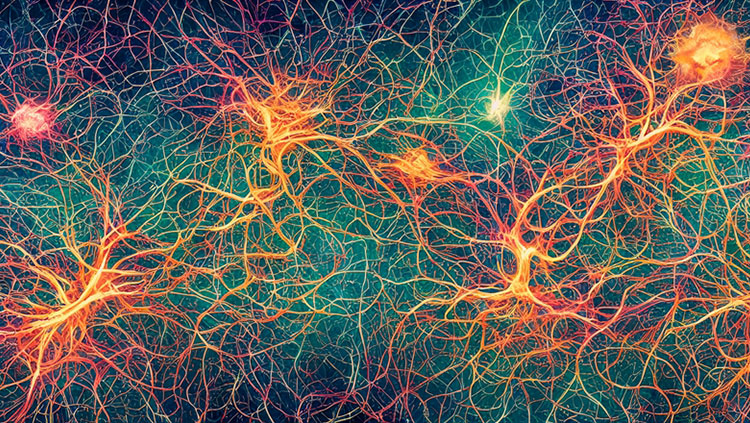
The term was also controversial. Whereas other diagnoses were based on clinicians’ observations and reports, “a major impetus for PTSD came from activists,” Friedman says. Findings from brain imaging technologies in the 1990s revealed the underlying neurobiology of PTSD and dispelled any doubts about the legitimacy of the diagnosis.
Intrusive recollections of a traumatic event — like flashbacks and nightmares — are a hallmark of PTSD. Some people are unable to recall details of the event, and they may have problems with memory and concentration in their daily lives. Several studies attribute this to shrinkage of the hippocampus, the region of the brain that directs the creation and storage of memories.
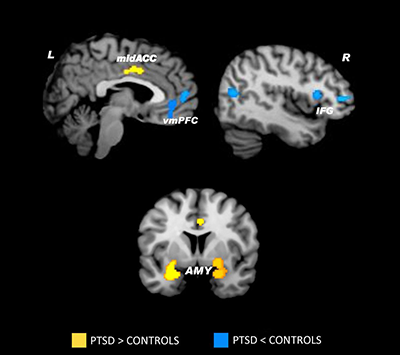
Fear is a learned response involving the amygdala, the brain’s emotional center that evaluates potential threats. In people with PTSD, this region is hyperreactive to reminders of the traumatic event and emotional stimuli like pictures of frightened faces. The degree of hyperactivity correlates with anxiety and symptom severity. The medial prefrontal cortex, a region in the front of the brain that acts like a braking system, normally tempers excessive activity in the amygdala. It helps us unlearn, or extinguish, fears when new information indicates we’re not in danger. But PTSD cuts the brakes: the medial prefrontal cortex is smaller, less active, and less able to restrain the amygdala’s fear response.
More Than Fear
For most people with PTSD, reminders of the trauma put their bodies on high alert. Their hearts race, and they feel anxious and afraid. A significant minority of patients don’t experience this. Instead, they experience dissociative states, where they feel detached from their emotions and perceive their surroundings are unreal. And, their brain activity is the inverse of the pattern typically seen in PTSD: they have an overactive prefrontal cortex and an underactive amygdala.
This suggested to neuroscientists that there were two distinct subtypes of PTSD — the classical presentation marked by flashbacks and intense fear, and the dissociative subtype where patients experience distortions in consciousness and perception. The DSM-5, published in 2013, makes this distinct by adding a dissociative subtype of PTSD.
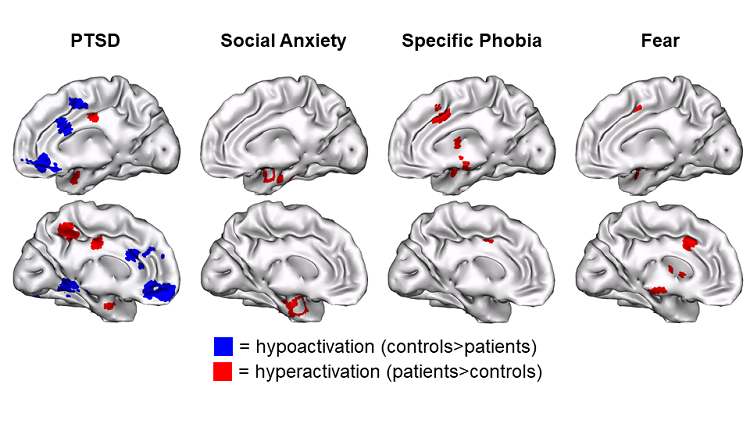
The DSM-5 also moved PTSD from the anxiety disorders to the newly created category of trauma and stressor related disorder. “I think we’ve really moved beyond fear and embraced the complexity of emotional response to trauma,” says Ruth Lanius, a psychiatrist and neuroscientist who studies PTSD. Her research in the early 2000s revealed the neural signature of dissociative PTSD and paved the way for its recognition as a distinct subtype.
Identifying and understanding all the subtypes of PTSD will help scientists and doctors tailor treatment to individuals.
Some scientists criticized the PTSD criteria in the DSM-5 for being overly complex — it includes 20 symptoms spread out across four symptom clusters. But, Friedman, who led the working group that revised the PTSD criteria for the DSM-5, believes “the reason we have all these symptoms is because we’re trying to cover a spectrum disorder with one diagnosis.”
When the first edition of the DSM was published in 1952, it included two subtypes of depression. The current edition of the DSM recognizes eight different kinds of depression. “I think PTSD is no different,” Friedman says. “We’re just starting a little later.”
This content was created with support from the Stanley Center for Psychiatric Research at Broad Institute.
CONTENTPROVIDEDBY
BrainFacts/SfN
References
Andreasen, N. C. (2010). Posttraumatic stress disorder: a history and a critique. Annals of the New York Academy of Sciences, 1208, 67–71. doi: 10.1111/j.1749-6632.2010.05699.x
Andreasen, N. C. (2011). What is post-traumatic stress disorder? Dialogues in Clinical Neuroscience, 13(3), 240–243. Retrieved from https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3182007/
Association, A. P. (2013). Posttraumatic Stress Disorder. In Diagnostic and Statistical Manual of Mental Disorders (DSM-5®) (5th ed.). American Psychiatric Pub.
Bremner, J. D. (1999). Acute and Chronic Responses to Psychological Trauma: Where Do We Go From Here? American Journal of Psychiatry, 156(3), 349–351. doi: 10.1176/ajp.156.3.349
Bremner, J. D., Randall, P., Scott, T. M., Bronen, R. A., Seibyl, J. P., Southwick, S. M., … Innis, R. B. (1995). MRI-Based Measurement of Hippocampal Volume in Patients With Combat-Related Posttraumatic Stress Disorder. The American Journal of Psychiatry, 152(7), 973–981. doi: 10.1176/ajp.152.7.973
Brewin, C. R. (2013). “I wouldn’t start from here”--an alternative perspective on PTSD from the ICD-11: comment on Friedman (2013). Journal of Traumatic Stress, 26(5), 557–559. doi: 10.1002/jts.21843
Crocq, M.-A., & Crocq, L. (2000). From shell shock and war neurosis to posttraumatic stress disorder: a history of psychotraumatology. Dialogues in Clinical Neuroscience, 2(1), 47–55. Retrieved from: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3181586/
Diagnostic and Statistical Manual of Mental Disorders. (1952).
Diagnostic and Statistical Manual of Mental Disorders (2nd ed.). (1968).
Diagnostic and Statistical Manual of Mental Disorders (3rd ed.). (1980).
Diagnostic and Statistical Manual of Mental Disorders (4th ed.). (1994).
Etkin, A., & Wager, T. D. (2007). Functional Neuroimaging of Anxiety: A Meta-Analysis of Emotional Processing in PTSD, Social Anxiety Disorder, and Specific Phobia. The American Journal of Psychiatry, 164(10), 1476–1488. doi: 10.1176/appi.ajp.2007.07030504
Francati, V., Vermetten, E., & Bremner, J. D. (2007). Functional neuroimaging studies in posttraumatic stress disorder: review of current methods and findings. Depression and Anxiety, 24(3), 202–218. doi: 10.1002/da.20208
Friedman, M. J. (2013). Finalizing PTSD in DSM-5: getting here from there and where to go next. Journal of Traumatic Stress, 26(5), 548–556. doi: 10.1002/jts.21840
Friedman, M. J. (2016, February 23). PTSD History and Overview. Retrieved from U.S. Department of Veterans Affairs website: https://web.archive.org/web/20180930130418/https://www.ptsd.va.gov/professional/ptsd-overview/ptsd-overview.asp
Friedman, M. J. (2017, May 31). History of PTSD in Veterans: Civil War to DSM-5. Retrieved from U.S. Department of Veterans Affairs website: https://www.ptsd.va.gov/understand/what/history_ptsd.asp
Gilbertson, M. W., Shenton, M. E., Ciszewski, A., Kasai, K., Lasko, N. B., Orr, S. P., & Pitman, R. K. (2002). Smaller hippocampal volume predicts pathologic vulnerability to psychological trauma. Nature Neuroscience, 5(11), 1242–1247. doi: 10.1038/nn958
Jones, E., Fear, N. T., & Wessely, S. (2007). Shell Shock and Mild Traumatic Brain Injury: A Historical Review. American Journal of Psychiatry, 164(11), 1641–1645. doi: 10.1176/appi.ajp.2007.07071180
Kilpatrick, D. G. (2013). The DSM-5 got PTSD right: comment on Friedman (2013). Journal of Traumatic Stress, 26(5), 563–566. doi: 10.1002/jts.21844
Lanius, R. A., Brand, B., Vermetten, E., Frewen, P. A., & Spiegel, D. (2012). The dissociative subtype of posttraumatic stress disorder: rationale, clinical and neurobiological evidence, and implications. Depression and Anxiety, 29(8), 701–708. doi: 10.1002/da.21889
Lanius, R. A., Vermetten, E., Loewenstein, R. J., Brand, B., Schmahl, C., Bremner, J. D., & Spiegel, D. (2010). Emotion modulation in PTSD: Clinical and neurobiological evidence for a dissociative subtype. The American Journal of Psychiatry, 167(6), 640–647. doi: 10.1176/appi.ajp.2009.09081168
Lanius, R., & Olff, M. (2017). The neurobiology of PTSD. European Journal of Psychotraumatology, 8(1). doi: 10.1080/20008198.2017.1314165
Shin, L. M., Rauch, S. L., & Pitman, R. K. (2006). Amygdala, medial prefrontal cortex, and hippocampal function in PTSD. Annals of the New York Academy of Sciences, 1071, 67–79. doi: 10.1196/annals.1364.007